The mediating effect of serum uric acid on the association of fat intake with renal dysfunction among Chinese adults
-
摘要:
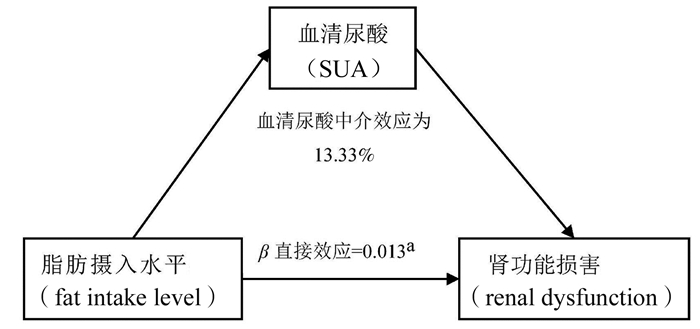
目的 探究血清尿酸(serum uric acid, SUA)在脂肪摄入水平与肾功能损伤关系中的中介效应。 方法 对来自2009年中国健康与营养调查(China Health and Nutrition Survey, CHNS)的8 187名具有完整血液检测信息的成人进行分析。肾功能损伤定义为肾小球滤过率(estimated glomerular filtration rate, eGFR)<60 ml/(min/1.73m2)。通过计算脂肪摄入量占总能量摄入量的百分比来评估脂肪摄入水平。使用基于二分类Logistic回归分析模型的限制性立方样条(restrictive cubic spline, RCS)探究脂肪摄入水平与肾功能损伤之间的剂量反应关系。采用Karlson-Holm-Breen分解方法中的Logistic回归进行中介分析。 结果 脂肪摄入水平与肾功能损伤呈线性正相关(β=0.015, 95% CI: 0.007~0.023, P < 0.001)。SUA的中介作用占脂肪摄入水平对肾功能损伤总效应的13.33%(P=0.014)。 结论 在中国成年人中,脂肪摄入水平增加可能会增加肾功能损伤的风险,其可能通过引起SUA水平升高而导致肾脏损害的发生。 Abstract:Objective To evaluate the association of high-fat diet with renal dysfunction and the mediating effect of serum uric acid. Methods Total 8 187 adult participants from the China Health and Nutrition Survey (CHNS) in 2009 with blood specimens were included in this national cross-sectional study. Renal dysfunction was defined as the estimated glomerular filtration rate (eGFR) < 60 ml/(min/1.73 m2). The fat intake level was assessed by the percentage of fat intake in total energy intake. Restrictive cubic spline (RCS) regression based on binary logistic regression analyses was used to explore the dose-response relationship between fat intake and renal dysfunction. Mediation analysis was conducted based on the Karlson-Holm-Breen method using Logistic regression. Results There was a linear positive relationship between fat intake level and the risk of renal dysfunction (β=0.015, 95% CI: 0.007-0.023, P < 0.001). The mediating effect of serum uric acid accounted for 13.33% of total effect of fat intake level on risk of renal dysfunction (P=0.014). Conclusions Increased fat intake level may increase the risk of renal dysfunction among Chinese adults, and serum uric acid may play a statistically significant mediatory role in the relationship between high-fat diet and renal dysfunction. -
Key words:
- Mediating effect /
- Serum uric acid /
- Fat intake level /
- Renal dysfunction /
- Chinese adults
-
表 1 不同脂肪摄入水平人群的一般特征[n(%)]
Table 1. Characteristics of subjects with different levels of fat intake [n(%)]
一般特征 脂肪摄入水平 χ2/F值 P值 低(n=2 047) 中(n=2 047) 中高(n=2 047) 高(n=2 046) 年龄(x±s,岁) 49.65±14.86 50.01±14.85 50.31±14.80 51.91±15.15 9.090a < 0.001 性别 15.349b 0.002 男 1 007(49.19) 999(48.80) 942(46.02) 898(43.89) 女 1 040(50.81) 1 048(51.20) 1 105(53.98) 1 148(56.11) 婚姻状况 16.617b 0.001 其他 305(14.90) 290(14.17) 310(15.14) 377(18.43) 已婚 1 742(85.10) 1 757(85.83) 1 737(84.86) 1 669(81.57) 受教育水平 135.933b < 0.001 小学及以下 1 022(49.93) 929(45.38) 798(38.98) 812(39.69) 中学 701(34.24) 671(32.78) 676(33.03) 643(31.43) 高中及以上 324(15.83) 447(21.84) 573(27.99) 591(28.88) 体育锻炼 MET(小时/周) 91.60 (22.17, 176.63) 83.17 (21.00, 169.00) 80.47 (21.00, 170.55) 55.79 (19.00, 147.00) 50.027c < 0.001 吸烟 从不吸烟 1 373(67.07) 1 359(66.39) 1 442(70.44) 1 455(71.11) 18.052b 0.006 过去吸烟 66(3.23) 73(3.57) 73(3.57) 59(2.88) 现在吸烟 608(29.70) 615(30.04) 532(25.99) 532(26.00) 饮酒 687(33.56) 690(33.71) 669(32.68) 642(31.38) 3.187b 0.364 每日总能量摄入(kcal) 2 051.40±650.19 2 143.12±626.84 2 136.90±626.97 2 194.94±647.47 17.780a < 0.001 每日蔬菜和水果摄入(g) 286.42±151.94 295.75±155.11 287.41±151.37 284.14±136.91 2.370a 0.069 每日嘌呤摄入量(mg/100 g) 346.29(233.74, 506.15) 428.66(290.85, 635.60) 488.59(322.42, 684.20) 526.16(370.10, 738.42) 518.440c < 0.001 BMI(kg/m2) 23.29±3.42 23.24±3.52 23.45±3.44 23.54±3.50 3.150a 0.024 高血压 595(29.07) 651(31.80) 633(30.92) 655(32.01) 5.177b 0.159 糖尿病 175(8.55) 190(9.28) 206(10.06) 242(11.83) 13.607b 0.003 高血脂 932(45.53) 1 004(49.05) 1 032(50.42) 1 108(54.15) 31.220b < 0.001 心脑血管疾病 33(1.61) 57(2.78) 52(2.54) 47(2.30) 6.948b 0.074 肾功能损伤 175(8.55) 244(11.92) 232(11.33) 321(15.69) 50.666b < 0.001 SUA(mg/dl) 5.10±1.85 5.21±1.79 5.14±1.67 5.30±1.80 4.900a 0.002 农村 1 588(77.58) 1 488(72.69) 1 354(66.15) 1 072(52.39) 332.528b < 0.001 城市化指数 54.72(42.81, 73.00) 61.02(50.40, 84.69) 68.94(54.95, 86.67) 81.93(57.13, 90.27) 638.368c < 0.001 注:a:单因素方差分析;b:Pearson χ2检验;c:Kruskal-Wallis检验。 表 2 SUA水平在脂肪摄入水平和肾功能损伤之间的中介效应
Table 2. The mediating effect of serum uric acid levels between fat intake and renal dysfunction
效应 β值 sx (95% CI)值 Z值 P值 中介作用
(%)总效应 0.015 0.004 (0.007~0.023) 3.60 < 0.001 直接效应 0.013 0.004 (0.005~0.021) 3.20 0.001 13.33 间接效应 0.002 0.001 (0.0003~0.003) 2.46 0.014 -
[1] Berger I, Wu S, Masson P, et al. Cognition in chronic kidney disease: a systematic review and meta-analysis[J]. BMC Med, 2016, 14(1): 206. DOI: 10.1186/s12916-016-0745-9. [2] Hill NR, Fatoba ST, Oke JL, et al. Global prevalence of chronic kidney disease - a systematic review and meta-analysis[J]. PLoS One, 2016, 11(7): e0158765. DOI: 10.1371/journal.pone.0158765. [3] Perlman RL, Finkelstein FO, Liu L, et al. Quality of life in chronic kidney disease (CKD): a cross-sectional analysis in the renal research Institute-CKD study[J]. Am J Kidney Dis, 2005, 45(4): 658-666. DOI: 10.1053/j.ajkd.2004.12.021. [4] Tanaka A, Taguchi I, Teraga WH, et al. Febuxostat does not delay progression of carotid atherosclerosis in patients with asymptomatic hyperuricemia: a randomized, controlled trial[J]. PLoS medicine, 2020, 17(4): e1003095. DOI: 10.1371/journal.pmed.1003095. [5] Toyama T, Furuichi K, Shimizu M, et al. Relationship between serum uric acid levels and chronic kidney disease in a japanese cohort with normal or mildly reduced kidney function[J]. PLoS One, 2015, 10(9): e0137449. DOI: 10.1371/journal.pone.0137449. [6] Tsai CW, Lin SY, Kuo CC, et al. Serum uric acid and progression of kidney disease: a longitudinal analysis and mini-review[J]. PLoS One, 2017, 12(1): e0170393. DOI: 10.1371/journal.pone.0170393. [7] Hossein RM, Mortazavi NM, Esmaillzadeh A, et al. Direct association between high fat dietary pattern and risk of being in the higher stages of chronic kidney disease[J]. Int J Vitam Nutr Res, 2019, 89(5-6): 261-270. DOI: 10.1024/0300-9831/a000260. [8] Rangel Silvares R, Nunes Goulart da Silva Pereira E, Eduardo Ilaquita Flores E, et al. High-fat diet-induced kidney alterations in rats with metabolic syndrome: endothelial dysfunction and decreased antioxidant defense[J]. Diabetes Metab Syndr Obes, 2019, 12(9): 1773-1781. DOI: 10.2147/DMSO.S211253. [9] Kuo CF, Grainge MJ, Zhang W, et al. Global epidemiology of gout: prevalence, incidence and risk factors[J]. Nat Rev Rheumatol, 2015, 11(11): 649-662. DOI: 10.1038/nrrheum.2015.91. [10] Zhang B, Zhai FY, Du SF, et al. The China Health and Nutrition Survey, 1989-2011[J]. Obes Rev, 2014, 15(Suppl 1): 2-7. DOI: 10.1111/obr.12119. [11] 王志宏, 张兵, 王惠君, 等. 中国成年人红肉摄人量对体重指数、体重及超重危险性影响的多水平纵向研究[J]. 中华流行病学杂志, 2013, 34(7): 661-667. DOI: 10.3760/cma.j.issn.0254-6450.2013.07.001.Wang ZH, Zhang B, Wang HJ, et al. Study on the multilevel and longitudinal association between red meat consumption and changes in body mass index, body weight and risk of incident overweight among Chinese adults[J]. Chin J Epidemiol, 2013, 34(7): 661-667. DOI: 10.3760/cma.j.issn.0254-6450.2013.07.001. [12] Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate[J]. Ann Intern Med, 2009, 150(9): 604-612. DOI: 10.7326/0003-4819-150-9-200905050-00006. [13] Webster AC, Nagler EV, Morton RL, et al. Chronic kidney disease[J]. Lancet, 2017, 389(10075): 1238-1252. DOI: 10.1016/S0140-6736(16)32064-5. [14] 杨月欣. 中国食物成分表标准版[M]. 第6版. 北京: 北京大学医学出版社, 2019.Yang YX. Chinese food composition table standard edition[M]. 6th ed. BeiJing: Peking University Medical Press, 2019. [15] Whitworth JA, Chalmers J. World health organisation-international society of hypertension (WHO/ISH) hypertension guidelines[J]. Clin Exp Hypertens, 2004, 26(7-8): 747-752. DOI: 10.1081/ceh-200032152. [16] Association AD. (2) Classification and diagnosis of diabetes[J]. Diabetes Care, 2017, 40(Suppl 1): S11. DOI: 10.2337/dc15-S005. [17] 诸骏仁, 高润霖, 赵水平, 等. 中国成人血脂异常防治指南(2016年修订版)[J]. 中国健康管理学杂志, 2017, 11(1): 7-28. DOI: 10.3760/cma.j.issn.0253-3758.2016.10.005.Zhu JR, Gao RL, Zhao SP, et al. Guidelines for prevention and Treatment of Dyslipidemia in Chinese Adults (2016 Revised Edition)[J]. Chin J Health Manage, 2017, 11(1): 7-28. DOI: 10.3760/cma.j.issn.0253-3758.2016.10.005. [18] Jones-Smith JC, Popkin BM. Understanding community context and adult health changes in China: development of an urbanicity scale[J]. Soc Sci Med (1982), 2010, 71(8): 1436-1446. DOI: 10.1016/j.socscimed.2010.07.027. [19] Kohler U, Karlson KB, Holm A. Comparing coefficients of nested nonlinear probability models[J]. Stata J, 2011, 11(3): 420-438. DOI: 10.1007/s00355-010-0469-2. [20] Song KK, Zhao DL, Wang YD, et al. Analysis of factors associated with death in maintenance hemodialysis patients: a multicenter study in China[J]. Chin Med J, 2017, 130(8): 885-891. DOI: 10.4103/0366-6999.204103. [21] Bach KE, Kelly JT, Palmer SC, et al. Healthy dietary patterns and incidence of CKD: a meta-analysis of cohort studies[J]. Clin J Am Soc Nephrol, 2019, 14(10): 1441-1449. DOI: 10.2215/CJN.00530119. [22] Yuzbashian E, Asghari G, Mirmiran P, et al. Associations of dietary macronutrients with glomerular filtration rate and kidney dysfunction: tehran lipid and glucose study[J]. J Nephrol, 2015, 28(2): 173-180. DOI: 10.1007/s40620-014-0095-7. [23] Decleves AE, Mathew AV, Cunard R, et al. AMPK mediates the initiation of kidney disease induced by a high-fat diet[J]. J Am Soc Nephrol, 2011, 22(10): 1846-1855. DOI: 10.1681/ASN.2011010026. [24] Trevisan R, Dodesini AR, Lepore G. Lipids and renal disease[J]. J Am Soc Nephrol, 2006, 17(4 Suppl 2): S145-S147. DOI: 10.1681/ASN.2005121320. [25] Lin ZJ, Zhang B, Liu XQ, et al. Abdominal fat accumulation with hyperuricemia and hypercholesterolemia quail model induced by high fat diet[J]. Chin Med Sci J, 2009, 24(3): 191-194. DOI: 10.1016/s1001-9294(09)60088-2. [26] Johnson RJ, Segal MS, Srinivas T, et al. Essential hypertension, progressive renal disease, and uric acid: a pathogenetic link?[J]. J Am Soc Nephrol, 2005, 16(7): 1909-1919. DOI: 10.1681/ASN.2005010063. [27] Liu H, Xiong J, He T, et al. High uric acid-induced epithelial-mesenchymal transition of renal tubular epithelial cells via the TLR4/NF-kB signaling pathway[J]. Am J Nephrol, 2017, 46(4): 333-342. DOI: 10.1159/000481668. [28] Vidon C, Boucher P, Cachefo A, et al. Effects of isoenergetic high-carbohydrate compared with high-fat diets on human cholesterol synthesis and expression of key regulatory genes of cholesterol metabolism[J]. Am J Clin Nutr, 2001, 73(5): 878-884. DOI: 10.1093/ajcn/73.5.878. [29] Bermúdez-López M, Arroyo D, Betriu à, et al. New perspectives on CKD-induced dyslipidemia[J]. Expert Opin Ther Targets, 2017, 21(10): 967-976. DOI: 10.1080/14728222.2017.1369961. -





 下载:
下载: