Association of systemic inflammatory response index and all-cause mortality in patients with cardiovascular and cerebrovascular diseases
-
摘要:
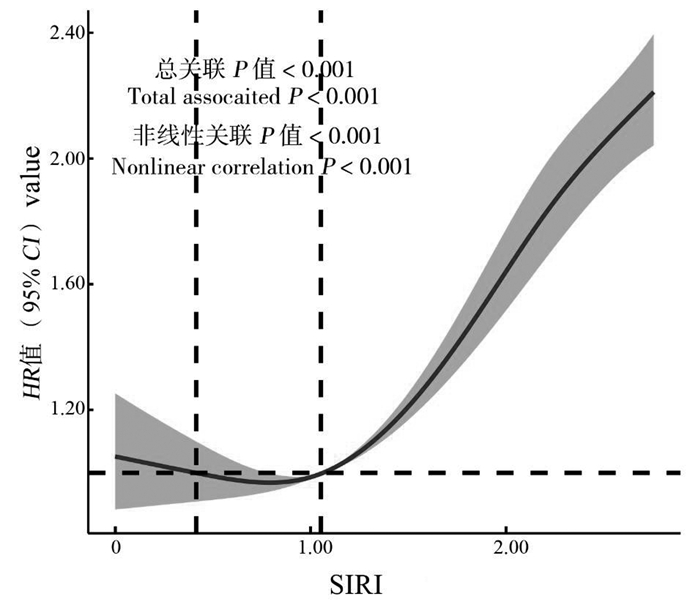
目的 分析一种新型炎症标志物——全身炎症反应指数(systemic inflammation response index, SIRI)与心脑血管疾病(cardiovascular and cerebrovascular diseases, CVD)患者全因死亡率之间的关系。 方法 基于英国生物样本库队列的数据,选择基线患有CVD的调查对象,共35 598名。利用限制性立方样条(restricted cubic splines, RCS)、Cox比例风险回归模型以及生存曲线研究SIRI与CVD患者全因死亡率之间的关系。通过时间依赖性受试者工作特征曲线分析,评估SIRI对患者生存的预测价值。根据种族、吸烟、饮酒等变量对数据进行亚组分析。 结果 随访时间为2010―2023年,5 755例CVD患者出现全因死亡。通过RCS分析发现,CVD患者的SIRI与全因死亡率之间呈“J”型非线性关联(P非线性 < 0.001),最适宜范围为0.79~1.05。SIRI高组(SIRI>1.05)相较于SIRI低组(SIRI≤1.05)的全因死亡风险增加49%(HR=1.49, 95% CI: 1.41~1.58)。与Q1组相比,Q3组的发病风险增加15%(HR=1.15, 95% CI: 1.06~1.26),Q4组的发病风险增加77%(HR=1.77, 95% CI: 1.63~1.92)。亚组分析结果表明,除年收入>100 000英镑的人群外,其他亚组中,SIRI高组比SIRI低组的全因死亡风险增加更明显,并且发现BMI与SIRI对全因死亡风险有交互作用。 结论 SIRI水平升高与CVD患者的全因死亡率增加相关,在随访时间为1年时SIRI高水平能更好地预测死亡风险。 Abstract:Objective The aim of this study was to analyse the relationship between a novel marker of inflammation, the systemic inflammatory response index (SIRI), and all-cause mortality in patients with cardiovascular and cerebrovascular diseases (CVD). Methods This study was based on data from the UK biobank cohort of 35 598 subjects selected for CVD at baseline. Restricted cubic spline, Cox regression model and survival curves were used to investigate the relationship between SIRI and all-cause mortality in patients with CVD. The predictive value of SIRI for patient survival was assessed by time-dependent receiver operating characteristic curve analysis. Data were analysed in subgroups according to variables such as race, smoking and alcohol consumption. Results A median follow-up period of 14.19 years revealed that 5 755 all-cause deaths occurred in patients with CVD. A significant J-shaped nonlinear relationship (Pnonlinear < 0.001) between SIRI and all-cause mortality in CVD patients was identified by restricted cubic spline (RCS) analysis, with an optimal range of 0.79-1.05. In patients with CVD, the high SIRI group (SIRI>1.05) exhibited a 49% elevated risk of all-cause mortality (HR=1.49, 95% CI: 1.41-1.58) in comparison to the low SIRI group (SIRI≤1.05). Furthermore, the Q3 group exhibited a 15% elevated risk of morbidity (HR=1.15, 95% CI: 1.06-1.26), while the Q4 group demonstrated a 77% increased risk of morbidity (HR=1.77, 95% CI: 1.63-1.92) in comparison to the Q1 group. The results of the subgroup analyses demonstrated a statistically significant increase in the risk of all-cause mortality in the high SIRI group relative to the low group across all different subgroups, with the exception of those with annual incomes greater than £100 000. Additionally, a significant interactive effect between BMI and SIRI on the risk of all-cause mortality was observed. Conclusions The results demonstrated a significant association between elevated levels of SIRI and an increased risk of mortality in patients with cardiovascular and CVD. Furthermore, elevated levels of SIRI were identified as a more accurate predictor of mortality risk at a follow-up period of one year. -
表 1 研究对象的基本特征
Table 1. Basic characteristics of the research object
变量
Variable总体
Total①生存
Survival①死亡
Death①P值
value总人数Total number 35 598 29 843 5 755 SIRI 1.21±0.63 1.16±0.60 1.48±0.72 < 0.001 淋巴细胞计数Lymphocyte count /(109 cells·L-1) 1.95±1.28 1.95±1.15 1.95±1.81 0.727 单核细胞计数Monocyte count/(109 cells·L-1) 0.51±0.24 0.50±0.22 0.57±0.34 < 0.001 中性粒细胞计数Neutrophil count/(109 cells·L-1) 4.39±1.51 4.29±1.42 4.89±1.81 < 0.001 随访时间/年Follow up time/year 13.47±2.79 14.44±0.83 8.44±3.82 < 0.001 年龄/岁Age/years 59.18±7.39 58.48±7.48 62.82±5.66 < 0.001 性别Gender 女Female 14 443(40.6) 12 901(43.2) 1 542(26.8) < 0.001 男Male 21 155(59.4) 16 942(56.8) 4 213(73.2) 种族Race 非白人Nonwhite 2 733(7.7) 2 323(7.8) 410(7.1) 0.090 白人White 32 865(92.3) 27 520(92.2) 5 345(92.9) 教育水平Educational level 高High 16 143(45.3) 14 079(47.2) 2 064(35.9) < 0.001 中Middle 9 575(26.9) 8 176(27.4) 1 399(24.3) 低Low 2 562(7.2) 2 093(7.0) 469(8.1) 其他Others 7 318(20.6) 5 495(18.4) 1 823(31.7) 年收入水平/英镑Income level/Pound <18 000 10 965(30.8) 8 250(27.6) 2 715(47.2) < 0.001 18 000~<31 000 9 817(27.6) 8 172(27.4) 1 645(28.6) 31 000~<52 000 8 247(23.2) 7 325(24.6) 922(16.0) 52 000~100 000 5 348(15.0) 4 950(16.6) 398(6.9) >100 000 1 221(3.4) 1 146(3.8) 75(1.3) TDI -1.17±3.15 -1.29±3.07 -0.53±3.44 < 0.001 吸烟状况Smoking status 从不Never 16 305(45.8) 14 483(48.5) 1 822(31.6) < 0.001 以前Before 15 418(43.3) 12 519(42.0) 2 899(50.4) 现在Current 3 875(10.9) 2 841(9.5) 1 034(18.0) 饮酒频率Drinking frequency 每天或几乎每天Every day or almost every day 7 741(21.8) 6 434(21.6) 1 307(22.7) < 0.001 3~4次/周3-4 times/week 7 915(22.2) 6 829(22.9) 1 086(18.9) 1~2次/周1-2 times/week 8 781(24.7) 7 504(25.1) 1 277(22.2) 1~3次/月1-3 times/month 3 838(10.8) 3 292(11.0) 546(9.5) 仅限特殊场合Special occasions only 4 139(11.6) 3 344(11.2) 795(13.8) 从不Never 3 184(8.9) 2 440(8.2) 744(12.9) IPAQ 低Low 7 274(20.4) 5 705(19.1) 1 569(27.3) < 0.001 中Middle 14 188(39.9) 11 920(40.0) 2 268(39.4) 高High 14 136(39.7) 12 218(40.9) 1 918(33.3) 饮食评分Diet score 2.50±1.25 2.52±1.25 2.37±1.26 < 0.001 BMI/(kg·m-2) 28.24±4.95 28.07±4.79 29.14±5.58 < 0.001 注:SIRI,全身炎症反应指数; TDI,汤森剥夺指数; IPAQ,国际体力活动问卷。
①以x±s或人数(占比/%)表示。
Note: SIRI, systemic inflammatory response index; TDI, Townsend deprivation index; IPAQ, international physical activity questionnaire.
① x±s or number of people (proportion/%).表 2 SIRI水平与心脑血管疾病患者全因死亡的Cox回归
Table 2. Cox regression analysis of SIRI levels and all-cause death in patients with cardiovascular and cerebrovascular diseases
变量
Variable模型1 Model 1① 模型2 Model 2① 模型3 Model 3① 连续型
ContinuityP值
valueHR值value
(95% CI)P值
valueHR值value
(95% CI)P值
valueHR值value
(95% CI)P值
valueSIRI 1.94(1.87~2.01) < 0.001 1.59(1.53~1.65) < 0.001 1.51(1.45~1.57) < 0.001 分组Group SIRI低组SIRI low group (≤1.05) 1.00 1.00 1.00 0.67(0.54~0.84) < 0.001 SIRI高组SIRI high group (>1.05) 2.09(1.97~2.20) < 0.001 1.58(1.50~1.68) < 0.001 1.49(1.41~1.58) < 0.001 1.61(1.52~1.70) < 0.001 Q1 1.00 1.00 1.00 0.44(0.28~0.68) < 0.001 Q2 1.17(1.07~1.28) 0.001 1.00(0.91~1.09) 0.960 0.96(0.88~1.05) 0.380 0.63(0.32~1.22) 0.168 Q3 1.61(1.48~1.75) < 0.001 1.22(1.12~1.33) < 0.001 1.15(1.06~1.26) 0.001 1.73(1.18~2.54) 0.005 Q4 2.95(2.74~3.19) < 0.001 1.96(1.81~2.12) < 0.001 1.77(1.63~1.92) < 0.001 1.55(1.41~1.70) < 0.001 注:SIRI,全身炎症反应指数。
①模型1未调整; 模型2调整了年龄、性别、种族、教育水平、年收入水平、汤森剥夺指数; 模型3在模型2基础上调整了BMI、吸烟状况、饮酒频率、身体活动和饮食评分。同时以SIRI为连续变量,在各组中进行Cox分析,该模型对年龄、性别、种族、教育水平、年收入水平、汤森剥夺指数、BMI、吸烟状况、饮酒频率、身体活动和饮食评分进行了校正。
Note: SIRI, systemic inflammatory response index.
① Model 1 unadjusted; Model 2 adjusted for age, sex, race, education level, annual income, and Townsend deprivation index; Model 3 adjusted for BMI, smoking status, drinking frequency, physical activity, and diet score on the basis of model 2. At the same time, the Cox analysis was carried out in each group with SIRI as a continuous variable. The model corrected for age, gender, race, education level, annual income, Townsend deprivation index, BMI, smoking status, drinking frequency, physical activity and diet score. -
[1] Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 study[J]. J Am Coll Cardiol, 2020, 76(25): 2982-3021. DOI: 10.1016/j.jacc.2020.11.010. [2] Center For Cardiovascular Diseases The Writing Committee Of The Report On Cardiovascular Health And Diseases In China N. Report on cardiovascular health and diseases in China 2023: an updated summary[J]. Biomed Environ Sci, 2024, 37(9): 949-992. DOI: 10.3967/bes2024.162. [3] Fearon WF, Fearon DT. Inflammation and cardiovascular disease: role of the interleukin-1 receptor antagonist[J]. Circulation, 2008, 117(20): 2577-2579. DOI: 10.1161/CIRCULATIONAHA.108.772491. [4] Casas R, Castro-Barquero S, Estruch R, et al. Nutrition and cardiovascular health[J]. Int J Mol Sci, 2018, 19(12): 3988. DOI: 10.3390/ijms19123988. [5] Haybar H, Shokuhian M, Bagheri M, et al. Involvement of circulating inflammatory factors in prognosis and risk of cardiovascular disease[J]. J Mol Cell Cardiol, 2019, 132: 110-119. DOI: 10.1016/j.yjmcc.2019.05.010. [6] 罗晓娟, 曾智. 全血细胞及分类计数在冠心病发生和预后预测中的作用研究进展[J]. 中国医刊, 2018, 53(3): 261-269. DOI: 10.3969/j.issn.1008-1070.2018.03.007.Luo XJ, Zeng Z. Research progress of effects of complete blood cells and classification counts on the occurrence and prognostic prediction of coronary heart diseases[J]. Chinese Journal of Medcine, 2018, 53(3): 261-269. DOI: 10.3969/j.issn.1008-1070.2018.03.007. [7] 梅超生, 闵轩. 血常规衍生复合炎症指标在冠心病患者中研究进展[J]. 中国心血管病研究, 2023, 21(12): 1145-1150. DOI: 10.3969/j.issn.1672-5301.2023.12.016.Mei CS, Min X. Advances in the study of routine blood-derived composite inflammatory indexes in patients with coronary artery disease[J]. Chin J Cardiovasc Res, 2023, 21(12): 1145-1150. DOI: 10.3969/j.issn.1672-5301.2023.12.016. [8] Li YY, Chen XF, Huang LZ, et al. Association between neutrophil-lymphocyte ratio and arterial stiffness in patients with acute coronary syndrome[J]. Biosci Rep, 2019, 39(5): BSR20190015. DOI: 10.1042/BSR20190015. [9] 金子奇. 系统性炎症与心脑血管疾病发病、全死因死亡风险的队列研究[D]. 杭州: 浙江大学, 2021.Jin ZQ. Cohort study on the relationship between systemic inflammation and the incidence of cardiovascular and cerebrovascular diseases and the risk of death from all causes[D]. Hangzhou: Zhejiang University, 2021. [10] Zhao SF, Dong SY, Qin YK, et al. Inflammation index SIRI is associated with increased all-cause and cardiovascular mortality among patients with hypertension[J]. Front Cardiovasc Med, 2023, 9: 1066219. DOI: 10.3389/fcvm.2022.1066219. [11] Sudlow C, Gallacher J, Allen N, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age[J]. PLoS Med, 2015, 12(3): e1001779. DOI: 10.1371/journal.pmed.1001779. [12] Zhang SY, Qian ZM, Chen L, et al. Erratum: exposure to air pollution during pre-hypertension and subsequent hypertension, cardiovascular disease, and death: a trajectory analysis of the UK biobank cohort[J]. Environ Health Perspect, 2023, 131(2): 29001. DOI: 10.1289/EHP12836. [13] Wang MY, Zhou T, Song QY, et al. Ambient air pollution, healthy diet and vegetable intakes, and mortality: a prospective UK Biobank study[J]. Int J Epidemiol, 2022, 51(4): 1243-1253. DOI: 10.1093/ije/dyac022. [14] Qi Q, Zhuang LP, Shen YH, et al. A novel systemic inflammation response index (SIRI) for predicting the survival of patients with pancreatic cancer after chemotherapy[J]. Cancer, 2016, 122(14): 2158-2167. DOI: 10.1002/cncr.30057. [15] Zhang Y, Liu FT, Wang Y. Evidence of the prognostic value of pretreatment systemic inflammation response index in cancer patients: a pooled analysis of 19 cohort studies[J]. Dis Markers, 2020, 2020: 8854267. DOI: 10.1155/2020/8854267. [16] McMaster WG, Kirabo A, Madhur MS, et al. Inflammation, immunity, and hypertensive end-organ damage[J]. Circ Res, 2015, 116(6): 1022-1033. DOI: 10.1161/CIRCRESAHA.116.303697. [17] Kong FL, Huang JH, Xu CH, et al. System inflammation response index: a novel inflammatory indicator to predict all-cause and cardiovascular disease mortality in the obese population[J]. Diabetol Metab Syndr, 2023, 15(1): 195. DOI: 10.1186/s13098-023-01178-8. [18] Wei L, Mao SQ, Liu XH, et al. Association of systemic inflammation response index with all-cause mortality as well as cardiovascular mortality in patients with chronic kidney disease[J]. Front Cardiovasc Med, 2024, 11: 1363949. DOI: 10.3389/fcvm.2024.1363949. [19] 唐锴, 刘磊, 谭震, 等. 外周血衍生炎症标志物SII和SIRI对急性心肌梗死患者院内不良心血管事件的预测价值[J]. 中国动脉硬化杂志, 2024, 32(7): 606-612. DOI: 10.20039/j.cnki.1007-3949.2024.07.008.Tang K, Liu L, Tan Z, et al. The predictive value of peripheral blood-derived inflammatory markers SII and SIRI for in-hospital adverse cardiovascular events in patients with acute myocardial infarc-tion[J]. Chin J Arterioscler, 2024, 32(7): 606-612. DOI: 10.20039/j.cnki.1007-3949.2024.07.008. [20] 刘艳华, 赵建全. 探讨SIRI、FIB-4对急性心肌梗死PCI术后患者不良预后的预测价值[J]. 内蒙古医学杂志, 2023, 55(12): 1432-1438. DOI: 10.16096/J.cnki.nmgyxzz.2023.55.12.005.Liu YH, Zhao JQ. To investigate the SIRI and fibrosis-4 index on the poor post-PCI patients with acute myocardial infarction predictive value of prognosis[J]. Inn Mong Med J, 2023, 55(12): 1432-1438. DOI: 10.16096/J.cnki.nmgyxzz.2023.55.12.005. [21] Qu C, Li X, Gao H. The impact of systemic inflammation response index on the prognosis of patients with ST-segment elevation myocardial infarction undergoing percutaneous coronary intervention[J]. Rev Cardiovasc Med, 2023, 24(5): 153. DOI: 10.31083/j.rcm2405153. [22] 高蓉蓉, 徐芳, 祝绪, 等. 全血细胞衍生的炎症标志物对急性心力衰竭患者的长期预后价值[J]. 临床心血管病杂志, 2022, 38(12): 980-987. DOI: 10.13201/j.issn.1001-1439.2022.12.010.Gao RR, Xu F, Zhu X, et al. Long-term prognostic value of whole blood cell-derived inflammatory markers in patients with acute heart failure[J]. J Clin Cardiol, 2022, 38(12): 980-987. DOI: 10.13201/j.issn.1001-1439.2022.12.010. [23] 尹玉莲, 戴朝晖, 李利, 等. 超声心动图参数联合系统性炎症反应指数对急性心力衰竭患者短期预后的预测价值[J]. 放射学实践, 2022, 37(9): 1166-1170. DOI: 10.13609/j.cnki.1000-0313.2022.09.020.Yin YL, Dai ZH, Li L, et al. Predictive value of ultrasonic cardiogram parameters combined with systemic inflammatory response index on short-term prognosis in patients with acute heart failure[J]. Radiol Pract, 2022, 37(9): 1166-1170. DOI: 10.13609/j.cnki.1000-0313.2022.09.020. [24] Zhou EY, Wu J, Zhou X, et al. Systemic inflammatory biomarkers are novel predictors of all-cause and cardiovascular mortality in individuals with osteoarthritis: a prospective cohort study using data from the NHANES[J]. BMC Public Health, 2024, 24(1): 1586. DOI: 10.1186/s12889-024-19105-5. [25] Peiseler M, Kubes P. More friend than foe: the emerging role of neutrophils in tissue repair[J]. J Clin Invest, 2019, 129(7): 2629-2639. DOI: 10.1172/JCI124616. [26] Liang X, Xiu CH, Liu MH, et al. Platelet-neutrophil interaction aggravates vascular inflammation and promotes the progression of atherosclerosis by activating the TLR4/NF-κB pathway[J]. J Cell Biochem, 2019, 120(4): 5612-5619. DOI: 10.1002/jcb.27844. [27] Nasir K, Guallar E, Navas-Acien A, et al. Relationship of monocyte count and peripheral arterial disease[J]. Arterioscler Thromb Vasc Biol, 2005, 25(9): 1966-1971. DOI: 10.1161/01.atv.0000175296.02550.e4. [28] Swirski FK, Nahrendorf M. Leukocyte behavior in atherosclerosis, myocardial infarction, and heart failure[J]. Science, 2013, 339(6116): 161-166. DOI: 10.1126/science.1230719. [29] Alebna PL, Mehta A, Yehya A, et al. Update on obesity, the obesity paradox, and obesity management in heart failure[J]. Prog Cardiovasc Dis, 2024, 82: 34-42. DOI: 10.1016/j.pcad.2024.01.003. [30] Lavie CJ, McAuley PA, Church TS, et al. Obesity and cardiovascular diseases: implications regarding fitness, fatness, and severity in the obesity paradox[J]. J Am Coll Cardiol, 2014, 63(14): 1345-1354. DOI: 10.1016/j.jacc.2014.01.022. -





 下载:
下载: