A cohort study on the relationship between women′s pre-pregnancy abnormal alanine aminotransferase, advanced age delivery and preterm low birth weight of newborns
-
摘要:
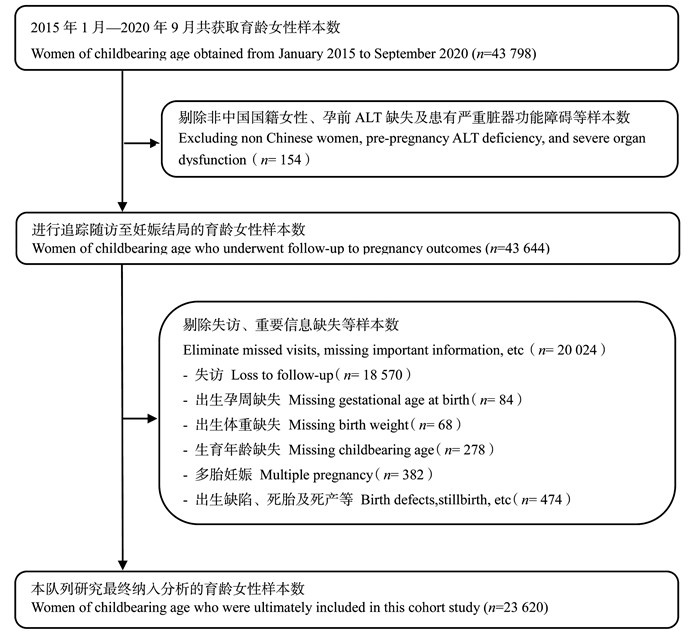
目的 探讨母亲孕前丙氨酸氨基转移酶(alanine aminotransferase, ALT)异常、高龄生育与新生儿早产低出生体重的关联。 方法 采用历史性队列研究,选取2015年1月―2020年9月在东莞市参加免费婚前健康检查和孕前优生健康检查项目的育龄女性,获取受检对象基本情况及相关检查结果,追踪随访获取其妊娠结局情况。采用多因素logistic回归分析母亲孕前ALT异常、高龄生育对新生儿早产低出生体重发生的影响,并进行亚组和敏感性分析检验结果的稳定性。 结果 共纳入23 620名母亲,新生儿早产低出生体重发生率为2.90%。多因素logistic回归分析结果显示,校正了协变量后母亲孕前ALT异常(RR=1.527, 95% CI: 1.133~2.016, P=0.004)、高龄生育(RR=1.257, 95% CI: 1.006~1.562, P=0.042)均可增加新生儿早产低出生体重发生风险。各亚组的效应值方向未发生改变,且组间异质性差异均无统计学意义(均P>0.05)。依次剔除了母亲孕前血糖(blood glucose, GLU)异常和孕前乙型肝炎表面抗原(hepatitis B surface antigen, HBsAg)阳性人群,效应值较为稳定。 结论 母亲孕前ALT异常和高龄生育与新生儿早产低出生体重相关。 Abstract:Objective To explore the relationship between women′s pre-pregnancy abnormal alanine aminotransferase(ALT), advanced age delivery and preterm low birth weight of newborns. Methods A historical cohort study was conducted to select women of childbearing age who participated in free pre-marital health check-ups and pre-pregnancy eugenic health check-ups in Dongguan from January 2015 to September 2020. The basic information and relevant examination results of the subjects were obtained, and their pregnancy outcomes were followed up. Multivariate logistic regressions were used to analyze the effects of women′s pre-pregnancy abnormal ALT and advanced age delivery on preterm low birth weight of newborns. The stability of the results was tested by subgroup analysis and sensitivity analysis. Results A total of 23 620 subjects were included in the analysis. The incidence of preterm low birth weight of newborns was 2.90%. Multivariate logistic regression analysis showed that after adjusting covariates, women′s pre-pregnancy abnormal ALT could increased the risk of preterm low birth weight (RR=1.527, 95% CI: 1.133-2.016, P=0.004). Delivery at an advanced age increased the risk of preterm low birth weight (RR=1.257, 95% CI: 1.006-1.562, P=0.042). Effect sizes were similar in subgroups of infant gender, mother′s delivery history and mode of delivery, and there was no statistically significant difference in heterogeneity between groups(all P>0.05). After excluding people with abnormal blood glucose(GLU) before pregnancy and hepatitis B surface antigen(HBsAg) positive before pregnancy, the effects remained. Conclusions Women′s pre-pregnancy abnormal ALT and advanced age delivery are associated with preterm low birth weight. -
Key words:
- Alanine aminotransferase /
- Advanced age /
- Delivery /
- Preterm birth /
- Birth weight /
- Cohort study
-
表 1 新生儿早产低出生体重影响因素
Table 1. The influencing factors of preterm low birth weight of newborns
特征Feature 总人数 ①Total ①(n=23 620) 早产低出生体重儿 ①Preterm low birth weight ①(n=684) χ2值value P值value 婴儿性别Infant gender 0.316 0.574 男Male 12 319(52.16) 349(2.83) 女Female 11 301(47.84) 335(2.96) 母亲民族Mother′s ethnic 0.004 0.949 汉族Han nationality 23 355(98.88) 677(2.90) 少数民族Minority nationality 265(1.12) 7(2.64) 母亲户口所在地Mother′s household registration location 0.802 0.371 本地市Local city 19 751(83.62) 581(2.94) 外地市Non local cities 3 869(16.38) 103(2.66) 母亲分娩史Mother′s delivery history 2.209 0.137 无None 13 069(55.33) 398(3.05) 有Had 10 551(44.67) 286(2.71) 孕前GLU异常Pre-pregnancy abnormal GLU 1.056 0.304 否No 21 971(93.02) 629(2.86) 是Yes 1 649(6.98) 55(3.34) 孕前HBsAg阳性Pre-pregnancy HBsAg positive 0.128 0.721 否No 22 025(93.25) 635(2.88) 是Yes 1 595(6.75) 49(3.07) 孕前ALT异常Pre-pregnancy abnormal ALT 9.597 0.002 否No 22 386(94.78) 630(2.81) 是Yes 1 234(5.22) 54(4.38) 分娩方式Delivery method 25.214 <0.001 阴道分娩Vaginal delivery 15 471(65.50) 386(2.50) 剖宫产分娩Cesarean section delivery 8 149(34.50) 298(3.66) 高龄生育Advanced age delivery 3.053 0.081 否No 19 562(82.82) 549(2.81) 是Yes 4 058(17.18) 135(3.33) 注:GLU, 血糖; HBsAg, 乙型肝炎表面抗原; ALT, 丙氨酸氨基转移酶。①以人数(占比/%)表示。
Note: GLU, blood glucose; HBsAg, hepatitis B surface antigen; ALT, alanine aminotransferase.①Number of people(proportion/%).表 2 母亲孕前ALT异常、高龄生育与新生儿早产低出生体重的关系
Table 2. Relationship between women′s pre-pregnancy abnormal ALT, advanced age delivery and preterm low birth weight of newborns
暴露因素Exposure factors 早产低出生体重Preterm low birth weight RR值 ① value ①(95% CI) P值 ① value ① aRR值value (95% CI) aP值value 孕前ALT异常Pre-pregnancy abnormal ALT 0.002 0.004 ② 否No 1.000 1.000 是Yes 1.580(1.177~2.079) 1.527 ②(1.133~2.016) 高龄生育Advanced age delivery 0.072 0.042 ③ 否No 1.000 1.000 是Yes 1.192(0.981~1.438) 1.257 ③(1.006~1.562) 注:GLU, 血糖; HBsAg, 乙型肝炎表面抗原; ALT, 丙氨酸氨基转移酶。①未校正;②校正了婴儿性别、母亲孕前HBsAg阳性、分娩方式、高龄生育、母亲分娩史、孕前GLU异常;③校正了婴儿性别、母亲孕前HBsAg阳性、分娩方式、孕前ALT异常、母亲分娩史、孕前GLU异常。
Note: GLU, blood glucose; H BsAg, hepatitis B surface antigen; ALT, alanine aminotransferase.① Not corrected; ② Corrected for infant gender, pre-pregnancy HBsAg positive of mother, delivery method, advanced age delivery, mother′s delivery history, and pre-pregnancy abnormal GLU; ③ Corrected for infant gender, pre-pregnancy HBsAg positive of mother, delivery method, pre-pregnancy abnormal ALT, mother′s delivery history, and pre-pregnancy abnormal GLU. -
[1] Mukherjee S, Shaw SC, Devgan A, et al. Survival and morbidities in very low birth weight (VLBW) infants in a tertiary care teaching hospital[J]. Int J Contemp Pediatr, 2017, 4(6): 2170-2174. DOI: 10.18203/2349-3291.ijcp20174751. [2] Chawanpaiboon S, Vogel JP, Moller AB, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis[J]. Lancet Glob Health, 2019, 7(1): e37-e46. DOI: 10.1016/S2214-109X(18)30451-0. [3] Khan MR, Maheshwari PK, Shamim H, et al. Morbidity pattern of sick hospitalized preterm infants in Karachi, Pakistan[J]. J Pak Med Assoc, 2012, 62(4): 386-388. [4] 冷俊宏, 王蕾棽, 李卫芹, 等. 孕早期谷丙转氨酶与发生巨大儿和大于胎龄儿关系[J]. 中国公共卫生, 2016, 32(7): 956-960. DOI: 10.11847/zgggws2016-32-07-21.Leng JH, Wang LS, Li WQ, et al. Association of maternal serum alanine aminotransferase in first trimester with risk of macrosomia and large for gestational age infant[J]. Chin J Public Health, 2016, 32(7): 956-960. DOI: 10.11847/zgggws2016-32-07-21. [5] Kaplan MM. Alanine aminotransferase levels: what's normal[J]. Ann Intern Med, 2002, 137(1): 49-51. DOI: 10.7326/0003-4819-137-1-200207020-00012. [6] 沈理笑. 早产低出生体重儿常见的生长发育问题及处理[J]. 中国实用儿科杂志, 2019, 34(10): 830-833. DOI: 10.19538/j.ek2019100608.Shen LX. Common growth and development problems of premature or low birth weight infants and the management[J]. Chin J Pract Pediatr, 2019, 34(10): 830-833. DOI: 10.19538/j.ek2019100608. [7] Genie YD, Kebede BF, Silesh Zerihun M, et al. Morbidity and mortality patterns of preterm low birthweight neonates admitted to referral hospitals in the Amhara region of Ethiopia: retrospective follow-up study[J]. BMJ Open, 2022, 12(7): e054574. DOI: 10.1136/bmjopen-2021-054574. [8] 庾静云, 何伟超, 刘建新, 等. 妇女孕前年龄、谷丙转氨酶及血糖水平与早产关系的队列研究[J]. 公共卫生与预防医学, 2020, 31(3): 108-111. DOI: 10.3969/j.issn.1006-2483.2020.03.026.Yu JY, He WC, Liu JX, et al. Cohort study on the relationship between women's pre-pregnancy age, alanine aminotransferase, blood glucose level and premature birth[J]. J Pub Health Preve Med, 2020, 31(3): 108-111. DOI: 10.3969/j.issn.1006-2483.2020.03.026. [9] 朱琳, 崔爱民, 成晓燕, 等. 35452例孕妇妊娠期肝功能异常与早产关系: 前瞻性队列研究[J]. 中国循证医学杂志, 2019, 19(4): 387-391. DOI: 10.7507/1672-2531.201810093.Zhu L, Cui AM, Cheng XY, et al. Liver dysfunction during pregnancy in 35 452 pregnancy women and its association with premature birth: a prospective cohort study[J]. Chin J Evid-Based Med, 2019, 19(4): 387-391. DOI: 10.7507/1672-2531.201810093. [10] 徐美珑, 毛金观, 李雁霞. 妊娠期ALT增高对新生儿出生体重的影响[J]. 中国优生与遗传杂志, 2000, (S1): 74. DOI: 10.13404/j.cnki.cjbhh.2000.s1.059.Xu ML, Mao JG, Li YX. Effect of increased ALT during pregnancy on newborn birth weight[J]. Chinese Journal of Birth Health & Heredity, 2000, (S1): 74. DOI: 10.13404/j.cnki.cjbhh.2000.s1.059. [11] 张金连, 苑东敏, 崔静, 等. 血清谷丙转氨酶水平与不同性别2型糖尿病患病的关系[J]. 现代预防医学, 2020, 47(8): 1514-1518. https://www.cnki.com.cn/Article/CJFDTOTAL-XDYF202008043.htmZhang JL, Yuan DM, Cui J, et al. Association of serum alanine aminotransferase level and type 2 diabetes mellitus in different genders[J]. Modern Preventive Medicine, 2020, 47(8): 1514-1518. https://www.cnki.com.cn/Article/CJFDTOTAL-XDYF202008043.htm [12] Kunutsor SK, Seddoh D. Alanine aminotransferase and risk of the metabolic syndrome: a linear dose-response relationship[J]. PLoS One, 2014, 9(4): e96068. DOI: 10.1371/journal.pone.0096068. [13] Tan PC, Aziz AZ, Ismail IS, et al. Gamma-glutamyltransferase, alanine transaminase and aspartate transaminase levels and the diagnosis of gestational diabetes mellitus[J]. Clin Biochem, 2012, 45(15): 1192-1196. DOI: 10.1016/j.clinbiochem.2012.05.025. [14] Tellapragada C, Eshwara VK, Bhat P, et al. Risk factors for preterm birth and low birth weight among pregnant Indian women: a hospital-based prospective study[J]. J Prev Med Public Health, 2016, 49(3): 165-175. DOI: 10.3961/jpmph.16.022. [15] 张言博, 赵志梅, 杨雪, 等. 妊娠期糖尿病对早产发生风险影响[J]. 中国公共卫生, 2019, 35(9): 1142-1145. DOI: 10.11847/zgggws1118703.Zhang YB, Zhao ZM, Yang X, et al. Association between gestational diabetes mellitus and risk of preterm birth[J]. Chin J Public Health, 2019, 35(9): 1142-1145. DOI: 10.11847/zgggws1118703. [16] Fuchs F, Monet B, Ducruet T, et al. Effect of maternal age on the risk of preterm birth: a large cohort study[J]. PLoS One, 2018, 13(1): e0191002. DOI: 10.1371/journal.pone.0191002. [17] 杨旻, 汪吉梅. 产妇年龄对新生儿不良结局影响的回顾性队列研究[J]. 中国循证儿科杂志, 2019, 14(4): 276-281. DOI: 10.3969/j.issn.1673-5501.2019.04.006.Yang M, Wang JM. Retrospective cohort study of the effect of maternal age on adverse neonatal outcomes[J]. Chin J Evid Based Pediatr, 2019, 14(4): 276-281. DOI: 10.3969/j.issn.1673-5501.2019.04.006. [18] 倪静宜, 陈林利, 陈丽菁, 等. 生育年龄与不良出生结局的关系及对适宜生育年龄的启示[J]. 现代预防医学, 2021, 48(20): 3720-3724, 3753. https://www.cnki.com.cn/Article/CJFDTOTAL-XDYF202120017.htmNi JY, Chen LL, Chen LJ, et al. Relationship between maternal age and adverse birth outcomes and inspiration for appropriate age of childbearing[J]. Modern Preventive Medicine, 2021, 48(20): 3720-3724, 3753. https://www.cnki.com.cn/Article/CJFDTOTAL-XDYF202120017.htm [19] Roustaei Z, Vehviläinen-Julkunen K, Tuomainen TP, et al. The effect of advanced maternal age on maternal and neonatal outcomes of placenta previa: a register-based cohort study[J]. Eur J Obstet Gynecol Reprod Biol, 2018, 227: 1-7. DOI: 10.1016/j.ejogrb.2018.05.025. [20] Oliveira LL, Goncalves AD, Costa JS, et al. Maternal and neonatal factors related to prematurity[J]. Rev Esc Enferm USP, 2016, 50(3): 382-389. DOI: 10.1590/S0080-623420160000400002. [21] 沈忠周, 王雅文, 马帅, 等. 新生儿早产、低出生体重及小于胎龄的危险因素[J]. 中华流行病学杂志, 2019, 40(9): 1125-1129. DOI: 10.3760/cma.j.issn.0254-6450.2019.09.020.Shen ZZ, Wang YW, Ma S, et al. Risk factors for preterm birth, low birth weight and small for gestational age: a prospective cohort study[J]. Chin J Epidemiol, 2019, 40(9): 1125-1129. DOI: 10.3760/cma.j.issn.0254-6450.2019.09.020. -





 下载:
下载: